Killer cell shift revealed
 Rogue immune cells linked to leukaemia appear to be a key driver of autoimmune diseases.
Rogue immune cells linked to leukaemia appear to be a key driver of autoimmune diseases.
A new Australian study has found gene variants associated with leukaemia can produce ‘rogue’ immune cells that drive autoimmune diseases.
Scientists had previously noticed that leukaemia patients were also likely to develop an autoimmune disease, such as rheumatoid arthritis or aplastic anaemia.
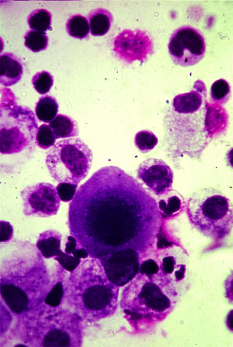
Research into this link revealed that immune cells called killer T cells - responsible for destroying harmful cells and pathogens - were a key player.
This new research provides insight into the role these killer T cells play in leukaemia and autoimmune disease, after scientists discovered gene variations affecting a protein that controls the growth of killer T cells can turn them rogue.
“We showed that these rogue killer T cells are driving the autoimmunity. They’re probably one of the cell types most directly contributing to autoimmune disease,” says Dr Etienne Masle-Farquhar, a postdoctoral researcher in the Immunogenomics and Genomic Medicine Labs at Garvan.
“Our research also narrows down a few pathways that might be helpful in targeting these cells for future treatments,” he says.
The findings are published in the journal, Immunity.
Cancers can grow when tumour cells are not identified or destroyed by the immune system. Autoimmune diseases occur when the immune system attacks the body’s own cells, mistaking them for harmful or foreign cells.
“We knew that people with various autoimmune diseases acquire these rogue killer T cells over time, but also that inflammation can cause immune cells to proliferate and develop mutations. We set out to discover whether the rogue T cells were causing these autoimmune conditions, or simply associated with them,” says Dr Masle-Farquhar.
The researchers used new high-resolution screening methods to look at blood from children with rare inherited autoimmune diseases.
They then used a technique called CRISPR/Cas9, a genome editing tool, in mouse models, to find out what happens when the protein STAT3 is genetically altered.
STAT3 is found throughout the body and is critical for various cell functions, including controlling the immune system’s B cells and T cells.
The team found that if these proteins are altered, they can cause rogue killer T cells to grow unchecked, resulting in enlarged cells that bypass immune checkpoints to attack the body’s own cells.
In addition, even just 1-2 per cent of a person’s T cells going rogue could cause autoimmune disease.
“It’s never been clear what the connection between leukaemia and autoimmune disease is – whether the altered STAT3 protein is driving disease, or whether leukaemic cells are dividing and acquiring this mutation just as a by-product. It’s a real chicken-and-egg question, which Dr Masle-Farquhar's work has been able to solve,” says Professor Chris Goodnow, Head of the Immunogenomics Lab and Chair of The Bill and Patricia Ritchie Foundation at Garvan.
“This gives some really good cracks in the coalface of where we might do better in terms of stopping these diseases, which are sometimes life threatening,” he says.
The team’s research may help develop screening technologies that clinicians could use to sequence the complete genome of every cell in a blood sample, to identify which cells might turn rogue and cause disease.








 Print
Print