Differences block path to help DCIS
 An Australian expert says the world needs better standards to reduce breast cancer mortality.
An Australian expert says the world needs better standards to reduce breast cancer mortality.
Variations in the treatment of DCIS (Ductal Carcinoma In Situ or precancerous cells of the breast) may be a contributing factor in worldwide differences in breast cancer mortality rates, according to Macquarie University’s Professor John Boyages.
The latest figures from the World Health Organisation show that Australia is still one of the best in the world at reducing the risk of dying from breast cancer.
But although breast cancer mortality rates in Australia fell by a staggering 35 per cent from 1989 until 2008, there has been no real change in the latest statistics published in December 2013.
In a new book, ‘DCIS of the Breast: Taking Control’, Professor Boyages summarises evidence and explains why he believes that if DCIS is left untreated, that for many patients, invasive cancer will occur given enough time.
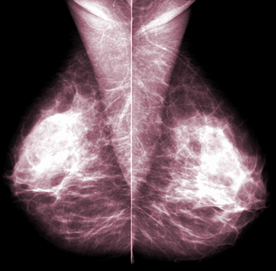
DCIS means that abnormal cells are lodged in one or more of the breast ducts, but have not yet escaped to potentially become breast cancer.
Professor Boyages calls this “precancer”.
“If you do not effectively diagnose and treat DCIS, there is no doubt in my mind, that for many patients, invasive breast cancer will occur given enough time,” he says.
“It is therefore vital for patients diagnosed with DCIS through mammography to understand their own risk, however low, of DCIS returning and the chance of it coming back as invasive breast cancer that may require more intensive treatments such as chemotherapy.”
Treating DCIS is controversial due to the diversity of medical opinion.
Professor Boyages says there is a lot of misinformation around about DCIS.
He says epidemiologists believe it is over-diagnosed and over-treated. On the other hand, treatment to the breast (lumpectomy, lumpectomy and radiation, mastectomy), lymph nodes (sample or not) and medications (tamoxifen or not) also varies widely.
In one study he quotes, 11 of the 29 patients (38 per cent) who did not have treatment of supposedly indolent low-grade DCIS, progressed to invasive cancer over a 30-year time period and six of the 11 died from it.
In a virtually unnoticed European clinical trial from September 2013, patients with DCIS treated by a lumpectomy had a 31 per cent recurrence in the breast within 15 years after surgery alone and half (15 per cent) of the recurrences were invasive.
Concerningly, by the 20 year point, four of every 10 patients with an invasive breast cancer recurrence had died from it.
“In my opinion, many of these deaths could have been prevented” Professor Boyages says.
DCIS of the Breast Taking Control is a 280 page full-colour, comprehensive guide for patients with DCIS and their caregivers, available online and at bookshops.
It addresses treatments, common side-effects, newer oncoplastic techniques, the role of sentinel node biopsy and tamoxifen and ways to cope with life after diagnosis, or if it reappears.








 Print
Print